Cortisol
I’ve spent a lot of time talking about the impact that food has on metabolic hormone balance, particularly insulin signaling. Food isn’t the only thing that can throw insulin out of balance. Stress is also a factor.
Cortisol is a glucocorticoid hormone, also known as our stress hormone. The body uses cortisol in preparation for the flight or fight emergency response. It does this by up regulating energy through the release of glucose and down regulating metabolic activity like digestion, reproduction and growth, things that aren’t necessary when you are running for your life.
In a perfect world, where stress is limited to short bursts during an emergency followed by long periods of calm and relaxation, the opposing effects of cortisol and insulin have a natural rhythm that create hormonal balance. Insulin stores energy, and when necessary cortisol moves that energy out of storage and burns it up during emergency action.
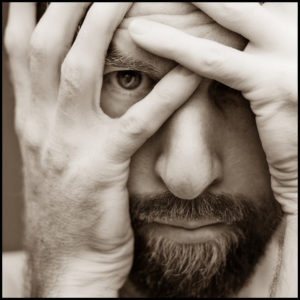 In our current society, stress is not fleeting it’s chronic. It can be emotional stress due to lifestyle factors or physical stress from injury or even psychological stress from something as common as lack of sleep. Chronically high levels of stress cause chronically high levels of cortisol. High levels of cortisol continually release stored glucose into the blood stream in preparation for the physical exertion that is expected from the flight or fight response. Without resolution to the stressor, or a burst of vigorous physical exertion the excess glucose being released doesn’t get burned up so blood glucose levels remain chronically high. Insulin is now required to move that glucose back into storage. In the face of chronic stress this process is like pushing glucose in through the front door not realizing the backdoor is wide open. Chronically high levels of cortisol lead to high levels of insulin.(1)
In our current society, stress is not fleeting it’s chronic. It can be emotional stress due to lifestyle factors or physical stress from injury or even psychological stress from something as common as lack of sleep. Chronically high levels of stress cause chronically high levels of cortisol. High levels of cortisol continually release stored glucose into the blood stream in preparation for the physical exertion that is expected from the flight or fight response. Without resolution to the stressor, or a burst of vigorous physical exertion the excess glucose being released doesn’t get burned up so blood glucose levels remain chronically high. Insulin is now required to move that glucose back into storage. In the face of chronic stress this process is like pushing glucose in through the front door not realizing the backdoor is wide open. Chronically high levels of cortisol lead to high levels of insulin.(1)
High cortisol causes high insulin and high insulin causes weight gain. Practical examples of high cortisol levels resulting in weight gain are Prednisone use and Cushing’s Disease. One study shows Prednisone use to increase insulin levels by 20% in healthy men.(2) Another study showed that long-term Prednisone use in transplant patients as an immunosuppressive therapy led to insulin resistance and even diabetes.(3) Long-term cortisol production, hypercortisolism is a diagnostic symptom of Cushing’s disease. People with Cushing’s disease, even mild forms of the disease gain weight.(4)
Lack of Sleep = High Insulin
Psycho logical stress due to sleep deprivation is something that many American’s suffer with. As with other forms of chronic stress, the stress due to sleep deprivation stimulates cortisol production. Sleep is an area of great interest and there are many studies showing the negative side effects of lack of sleep. A single night with no sleep caused an increase in cortisol levels by 100% and by the next night cortisol was still about 40% higher than normal.(5)(6) A night of only 4 hours of sleep has been shown to decrease insulin sensitivity by 40%. (7) In only 5 days of restricted sleep (4 hours in bed) there was a 25% decrease in insulin sensitivity.(8) Less than 8 hours of sleep was proportionally related to increased BMI in participants in the Wisconsin Sleep Cohort Study. Leptin was also reduced by 15.5% with just a three-hour reduction in sleep from 8 hours to 5 hours and 15% higher ghrelin for the same three-hour reduction. This translates to an increase in appetite and hunger and a decrease in digestion potentially resulting in weight gain and contributing to obesity.(9)
logical stress due to sleep deprivation is something that many American’s suffer with. As with other forms of chronic stress, the stress due to sleep deprivation stimulates cortisol production. Sleep is an area of great interest and there are many studies showing the negative side effects of lack of sleep. A single night with no sleep caused an increase in cortisol levels by 100% and by the next night cortisol was still about 40% higher than normal.(5)(6) A night of only 4 hours of sleep has been shown to decrease insulin sensitivity by 40%. (7) In only 5 days of restricted sleep (4 hours in bed) there was a 25% decrease in insulin sensitivity.(8) Less than 8 hours of sleep was proportionally related to increased BMI in participants in the Wisconsin Sleep Cohort Study. Leptin was also reduced by 15.5% with just a three-hour reduction in sleep from 8 hours to 5 hours and 15% higher ghrelin for the same three-hour reduction. This translates to an increase in appetite and hunger and a decrease in digestion potentially resulting in weight gain and contributing to obesity.(9)
Meditation For Stress Management
Managing stress is an important lifestyle factor for everyone but it’s particularly important if you are trying to lose weight and regain health. Managing insulin through food choices is huge but it won’t solve the whole problem. Stress must be managed.
There are many ways to manage stress. Things that work for one person may not work for another. It’s important to figure out what works for you. One thing that seems to be universally accepted for stress management is meditation. If you haven’t tried it you should. You could look for meditation centers in your area and sign up for a beginner class to get started. There are also CDs and DVDs that will walk you through guided meditation. One of my new favorite things is an app called Headspace. Headspace has a free 10 day trial that introduces you to mediation. Give it a try, you might just like it.
Eat well, feel good, have fun!
References:
- Rosmond, R. (1998). Stress-Related Cortisol Secretion in Men: Relationships with Abdominal Obesity and Endocrine, Metabolic and Hemodynamic Abnormalities. Journal of Clinical Endocrinology & Metabolism, 83(6), 1853-1859. doi:10.1210/jc.83.6.1853
- Pagano, G., Cavallo-Perin, P., Cassader, M., Bruno, A., Ozzello, A., Masciola, P., … Imbimbo, B. (1983). An in vivo and in vitro study of the mechanism of prednisone-induced insulin resistance in healthy subjects. Journal of Clinical Investigation, 72(5), 1814-1820. doi:10.1172/jci111141
- Gomes, M. B., & Cobas, R. A. (2009). Post-transplant diabetes mellitus. Diabetol Metab Syndr,1(1), 14. doi:10.1186/1758-5996-1-14
- Tauchmanovà, L., Rossi, R., Biondi, B., Pulcrano, M., Nuzzo, V., Palmieri, E., … Lombardi, G. (2002). Patients with Subclinical Cushing’s Syndrome due to Adrenal Adenoma Have Increased Cardiovascular Risk. The Journal of Clinical Endocrinology & Metabolism,87(11), 4872-4878. doi:10.1210/jc.2001-011766
- Joo, E. Y., Yoon, C. W., Koo, D. L., Kim, D., & Hong, S. B. (2012). Adverse Effects of 24 Hours of Sleep Deprivation on Cognition and Stress Hormones. J Clin Neurol, 8(2), 146. doi:10.3988/jcn.2012.8.2.146
- Leproult, R., Copinschi, G., Buxton, O., & Van Cauer, E. (1997). Sleep loss results in an elevation of cortisol levels the next evening. Sleep, 10, 865-70. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/9415946
- Spiegel, K. (2005). Sleep loss: a novel risk factor for insulin resistance and Type 2 diabetes.Journal of Applied Physiology, 99(5), 2008-2019. doi:10.1152/japplphysiol.00660.2005
- Rao, M. N., Neylan, T. C., Grunfeld, C., Mulligan, K., Schambelan, M., & Schwarz, J. (2015). Subchronic Sleep Restriction Causes Tissue-Specific Insulin Resistance. The Journal of Clinical Endocrinology & Metabolism, 100(4), 1664-1671. doi:10.1210/jc.2014-3911
- Taheri, S., Lin, L., Austin, D., Young, T., & Mignot, E. (2004). Short Sleep Duration Is Associated with Reduced Leptin, Elevated Ghrelin, and Increased Body Mass Index.PLoS Med, 1(3), e62. doi:10.1371/journal.pmed.0010062

I’m Amy a board certified holistic nutritionist, certified functional nutritionist and lifestyle practitioner and certified Life Coach. I help women in midlife understand the changing needs of their body so that they can stop dieting and lose weight permanently. At 56 I live what I teach. Don’t believe the story that your best years are behind you. They are not. Your best years are just starting!


